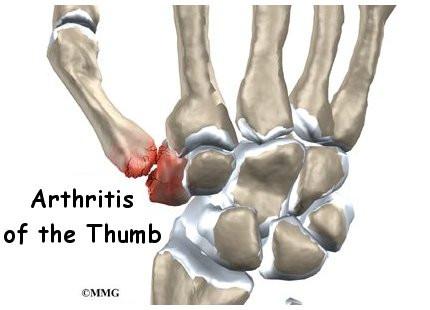
Base of thumb arthritis is a common, painful condition causing pain in the base of the thumb. There are two joints in the area that can be affected, and treatment depends on the degree to which these are affected. Many people have changes in these joints, and may not realise it. Accidents such as motor vehicle accidents, falls, workplace incidents may all flare up previously non painful disease and cause ongoing pain.
The mainstay of treatment is actually not surgery. Non surgical management is often very effective, and over time symptoms can settle. All patients in my practise go through a period of non surgical management before considering surgery.
Non surgical management consists of:
- Analgesia – use of analgesics such as paracetamol regularly is very effective. Many people consider paracetamol to not be effective treating pain, and certainly when pain is severe its not. However it is great at preventing pain from escalating, but needs to be taken regularly to be effective.
- Splinting – A thumb splint may be awkward to wear, but it will prevent flare ups after heavy activity. I typically advise not wearing it during normal activities as it will cause stiffness and loss of strength.
- Steroid injections – A mainstay of treatment. Steroid injections are usually very effective. I refer you to a radiologist to have these performed under ultrasound guidance to ensure they are in the correct joint. The steroid only works in the location it is injected. If more than one joint is involved (the CMCJ and STT) then you may require two injections to be effective. I consider this effective if the results last at least 3 months.
If non surgical management fails, surgery is available and is a great way of relieving pain. There are always downsides to surgery however.
There are many, many ways to surgically treat base of thumb arthritis. There are three main methods I consider to be the most effective.
- Joint de-innervation – A procedure where the fibres to the joint that carry pain are targeted. Sensation to the skin is not altered. This is a good option for those unable to afford the time to recover from other procedures. Recovery is typically in a number of weeks. Due to the diffuse nature in which pain fibres reach the joint, success is variable however. I typically quote success rates of 60%, i.e. 4 in 10 will have no benefit. In the cases of failure however, all other options are still available.
- Trapeziectomy – Is a procedure where the trapezium (bone) is excised. A slip of tendon is used to suspend the base of the thumb. This is the classic “gold standard”of thumb arthritis treatment and really the only option if both joints of the thumb (CMCJ and STT) are involved.
- Joint replacement – Is a procedure where the CMC joint of the thumb is replaced with a prosthetic device. Classically many devices have been tried and all failed or gave poor results. I use the Arpe prosthesis which has been in use in Europe for over 10 years now. Its retention rate is 94% over 10 years (compared to a hip prosthesis at 93%) and has in my experience given excellent results. It is my preferred treatment for isolated CMCJ arthritis.